Obsessive-Compulsive Disorder is a complex and challenging condition that affects millions of people worldwide. Understanding OCD is the first step in helping those who suffer from it. With appropriate treatment, individuals with OCD can learn to manage their symptoms, reduce the impact of the disorder on their lives, and lead fulfilling and productive lives. Early intervention and a combination of therapies can make a significant difference in the outcome for those struggling with OCD.
What is OCD
Obsessive-compulsive disorder (OCD) is a long-lasting disorder in which a person experiences uncontrollable and recurring thoughts (obsessions), engages in repetitive behaviors (compulsions), or both. People with OCD have time-consuming symptoms that can cause significant distress or interfere with daily life. However, treatment is available to help people manage their symptoms and improve their quality of life.
Is OCD an anxiety disorder?

OCD used to be classified as an anxiety disorder. But that changed with the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders, published in 2013. It’s now in a category called “Obsessive-Compulsive and Related Disorders.” However, most people with OCD also have an anxiety disorder.
What are the signs and symptoms of OCD?

People with OCD may have obsessions, compulsions, or both. Obsessions are repeated thoughts, urges, or mental images that are intrusive, unwanted, and make most people anxious. Common obsessions include:
- Fear of germs or contamination
- Fear of forgetting, losing, or misplacing something
- Fear of losing control over one’s behavior
- Aggressive thoughts toward others or oneself
- Unwanted, forbidden, or taboo thoughts involving sex, religion, or harm
- Desire to have things symmetrical or in perfect order
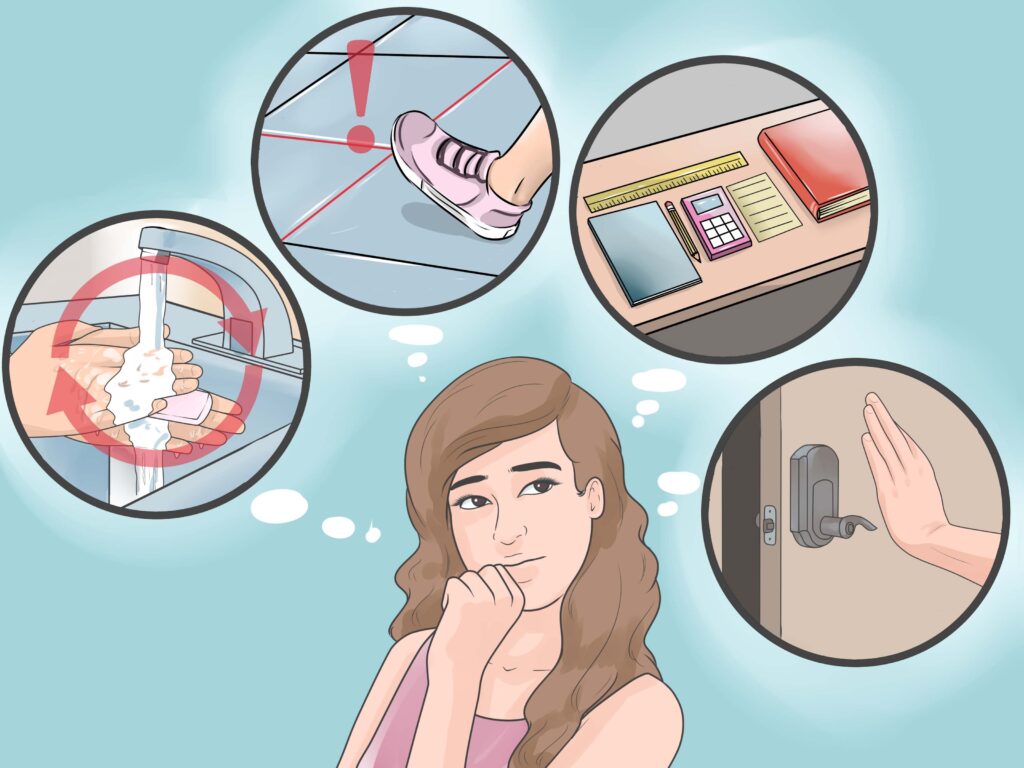
Compulsions are repetitive behaviors a person feels the urge to do, often in response to an obsession. Common compulsions include:
- Excessive cleaning or handwashing
- Ordering or arranging items in a particular, precise way
- Repeatedly checking things, such as that the door is locked or the oven is off
- Compulsive counting
- Praying or repeating words silently
Not all repeated thoughts are obsessions, and not all rituals or habits are compulsions. However, people with OCD generally:
- Can’t control their obsessions or compulsions, even when they know they’re excessive.
- Spend more than 1 hour a day on their obsessions or compulsions.
- Don’t get pleasure from their compulsions but may feel temporary relief from their anxiety.
- Experience significant problems in daily life due to these thoughts or behaviors.
- Some people with OCD also have a tic disorder involving repetitive movements or sounds.
- Motor tics are sudden, brief, repetitive movements, such as eye blinking and other eye movements, facial grimacing, shoulder shrugging, and head or shoulder jerking.
- Vocal tics include things like repetitive throat-clearing, sniffing, or grunting sounds.
- It is common for people with OCD to also have a diagnosed mood disorder or anxiety disorder.
OCD symptoms may begin anytime but usually start between late childhood and young adulthood. Most people with OCD are diagnosed as young adults. The symptoms of OCD may start slowly and can go away for a while or worsen as time passes. During times of stress, the symptoms often get worse. A person’s obsessions and compulsions also may change over time.
People with OCD might avoid situations that trigger their symptoms or use drugs or alcohol to cope. Many adults with OCD recognize that their compulsive behaviors do not make sense. However, children may not realize that their behavior is out of the ordinary and often fear that something terrible will happen if they do not perform certain compulsive rituals.
Causes of obsessive compulsive disorder

It’s not clear what causes OCD. A number of different factors may play a part, including:
family history : you’re more likely to develop OCD if a family member has it. It may be learned behaviour, or possibly because of your genes differences in the brain. some people with OCD have areas of unusually high activity in their brain or low levels of a chemical called serotonin
life events: OCD may be more common in people who have been bullied, abused or neglected, and it sometimes starts after an important life event, such as childbirth or a bereavement personality
neat, meticulous, methodical people with high personal standards may be more likely to develop OCD, also people who are generally quite anxious or have a very strong sense of responsibility for themselves and others
Impact on Daily Life

OCD can have a profound impact on a person’s quality of life. The disorder can consume a significant amount of time, making it difficult to engage in daily activities, maintain relationships, or perform well at work or school. The constant need to perform compulsions can be exhausting, and the persistent obsessions can lead to overwhelming anxiety and emotional distress. In some cases, individuals with OCD may avoid certain places, people, or situations that trigger their obsessions, leading to social isolation or difficulties in maintaining employment or education. The disorder can also contribute to the development of other mental health issues, such as depression or substance abuse.
Treatment

Patients with OCD who receive appropriate treatment commonly experience increased quality of life and improved functioning. Treatment may improve an individual’s ability to function at school and work, develop and enjoy relationships, and pursue leisure activities.
Cognitive Behavioral Therapy
One effective treatment is a type of cognitive-behavioral therapy (CBT) known as exposure and response prevention (ERP). During treatment sessions, patients are exposed to feared situations or images that focus on their obsessions. Although it is standard to start with those that only lead to mild or moderate symptoms, initially the treatment often causes increased anxiety. Patients are instructed to avoid performing their usual compulsive behaviors (known as response prevention). By staying in a feared situation without anything terrible happening, patients learn that their fearful thoughts are just thoughts. People learn that they can cope with their thoughts without relying on ritualistic behaviors, and their anxiety decreases over time.
Using evidence-based guidelines, therapists and patients typically collaborate to develop an exposure plan that gradually moves from lower anxiety situations to higher anxiety situations.
Exposures are performed both in treatment sessions and at home. Some people with OCD may not agree to participate in CBT because of the initial anxiety it evokes, but it is the most powerful tool available for treating many types of OCD.
Medication
A class of medications known as selective serotonin reuptake inhibitors (SSRIs), typically used to treat depression, can also be effective in the treatment of OCD. The SSRI dosage used to treat OCD is often higher than that used to treat depression. Patients who do not respond to one SSRI medication sometimes respond to another.
The maximum benefit usually takes six to twelve weeks or longer to be fully visible. Patients with mild to moderate OCD symptoms are typically treated with either CBT or medication depending on patient preference, the patient’s cognitive abilities and level of insight, the presence or absence of associated psychiatric conditions, and treatment availability.
The best treatment of OCD is a combination of CBT and SSRIs, especially if OCD symptoms are severe.
Neurosurgical treatment
Some newer studies show that gamma ventral capsulotomy, a surgical procedure, can be very effective for patients who do not respond to typical treatments and are very impaired, but it is underused due to historical prejudice and its invasiveness.
Deep brain stimulation, which involves an implanted device in the brain, has data to support efficacy and does not permanently destroy brain tissue as done in a capsulotomy. However, it is still highly invasive and complex to manage, and there are limited providers and hospital systems trained to offer this treatment and, able to provide the long-term support needed by DBS patients.













Leave a comment